In Indiana, documentation of caregiver training is not optional — it is a compliance requirement under both state law and federal Conditions of Participation. Agencies must not only train caregivers in CPR, AED, and First Aid, but also retain documentation that demonstrates the training meets regulatory expectations.
Indiana Administrative Code Requirements
State regulations require that all personnel records for employees delivering home health services include documentation of current qualifications and certifications. Specifically:
-
Under 410 IAC 17-12-1, agencies must maintain personnel records that include copies of current licenses, certifications, or registrations required to perform the service (such as CPR/AED/First Aid) and keep them current and accessible. Legal Information Institute
-
Further, 410 IAC 17-14-1 sets a framework for training requirements and continuing education programs for home health aides, and puts the onus on agencies to maintain sufficient documentation demonstrating caregiver competency and training completion prior to patient contact. Legal Information Institute
Though Indiana’s administrative code does not list CPR/AED specifically in every section of the home health aide competency requirements, the regulatory language on personnel qualifications and documentation applies broadly to all required competencies, including emergency response capabilities.
Federal Requirements Under 42 CFR
At the federal level, agency compliance obligations are set out in 42 CFR Part 484, the Conditions of Participation (CoPs) for Home Health Agencies. While 42 CFR does not explicitly list CPR/AED as individual training topics, it requires that agencies:
-
Train home health aides and demonstrate competence in tasks before allowing them to perform those tasks independently. Aides must not be considered competent in any task for which they have been rated “unsatisfactory” until they have received training and passed evaluation. Agencies must maintain documentation showing these standards have been met. ecfr.gov+1
-
Provide annual in-service training of at least 12 hours per 12-month period for home health aides, with documentation of completion maintained by the agency. ecfr.gov
These federal requirements make it clear that documented competency evaluation and training records are expected for all care tasks — especially emergency preparedness tasks such as CPR, AED use, and First Aid.
Why This Matters for CPR/AED/First Aid
Regulators and surveyors interpret these standards to mean that a home health agency must be able to produce records showing:
-
Caregivers hold current CPR/AED/First Aid cards from a recognized training provider (such as the American Heart Association).
-
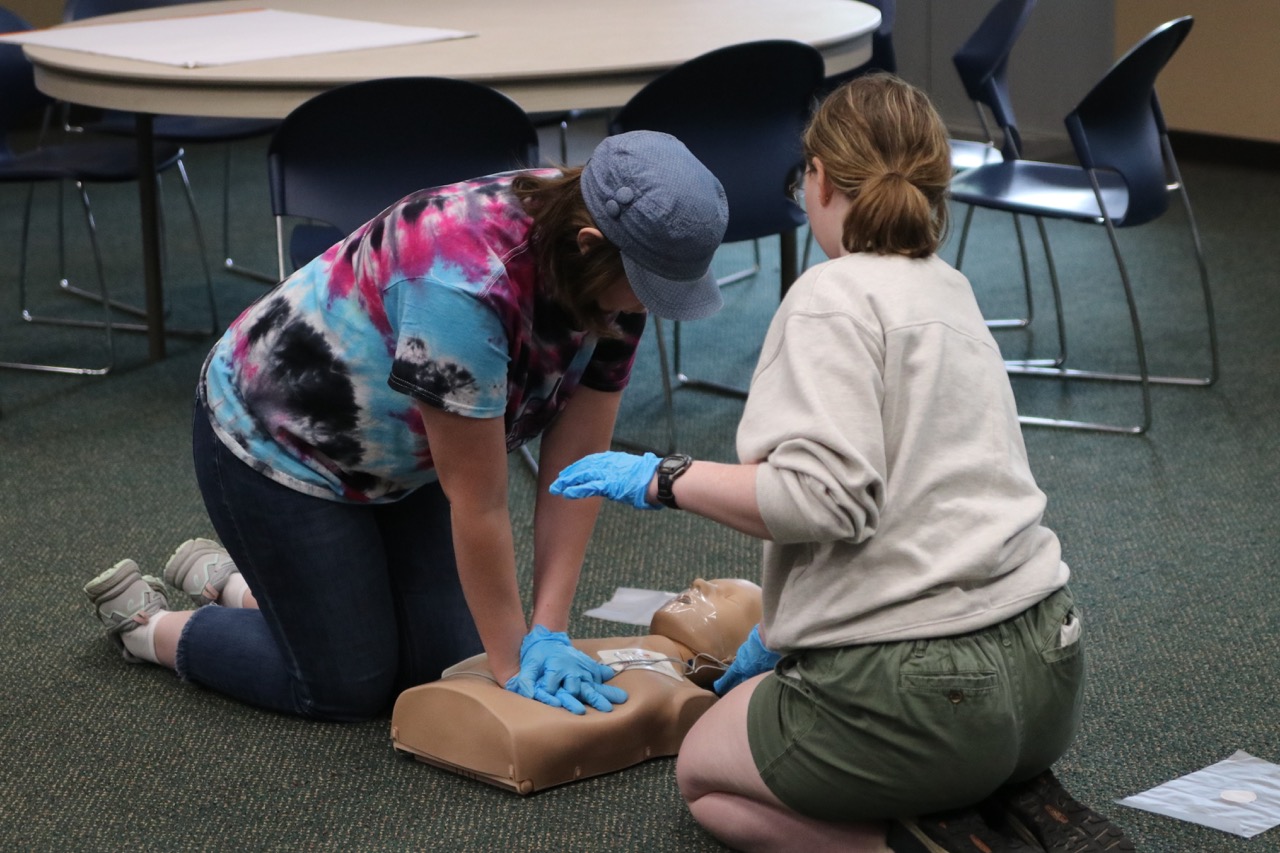
Training includes hands-on skills verification, not just online completion.
-
Annual in-service or refresher training is documented in personnel files.
-
Agencies track expiration dates and recertification statuses.
If an agency cannot produce these records during a licensure survey or audit, it can lead to survey deficiencies or corrective action requirements.
How RESQ & Arise Ensures You Meet These Exact Requirements
At RESQ & Arise Safety and CPR Training, we support Indiana home health agencies with training programs designed explicitly to satisfy both state personnel documentation expectations and federal competency standards:
-
Training certificates that clearly document completion and expiration dates for inclusion in personnel files.
-
Annual refresher and in-service options to support compliance with 42 CFR in-service requirements.
-
Clear documentation packages you can use for your internal files or survey responses.
Our training programs are tailored for agencies that need to demonstrate compliance under 410 IAC 17 and 42 CFR Part 484, and we help you maintain audit-ready records every step of the way.
Let RESQ & Arise help you build a compliant, confident caregiving workforce — so you never have to worry about documentation gaps when it matters most.